By Kate S. KuKanich, DVM, PhD, Diplomate ACVIM, Kansas State
University
PROFILE
Defintion
A urinary tract infection (UTI) occurs when a bacterium, such as
uropathogenic
Escherichia coli, overcomes host defenses and
adheres to, multiplies, and persists in the urinary tract.
► These infections involve the bladder and are
typically initial infections with no concurrent disease or
underlying structural or functional abnormality (ie, no compromise
of host defense mechanisms).
► These infections are associated with
pyelonephritis, prostatitis, concurrent systemic diseases (diabetes
mellitus, hyper-adrenocorticism), and either systemic
(corticosteroid use) or local (indwelling urinary catheter, uroliths,
neoplasia) alterations in immunity through compromised host defense
mechanisms.
Incidence/Prevalence
- E coli is the most common bacterium isolated in
canine and feline UTIs.1,2
- Approximately 14% of dogs have UTI during their lifetime,
but young, healthy cats have an innate resistance and rarely
develop UTI.3
Signalment
- Age
► Dogs may have UTI at any age.
► Cats older than 10 years of age are predisposed and usually
have concurrent illness.
► Female dogs are at increased risk for UTI
due to easier ascension of bacteria through a shorter urethra. In
male dogs, UTI is generally classified as complicated.
Causes
- E coli, a gram-negative bacterium, has been
isolated in 44% of all canine UTIs and in as many as 67% of
feline UTIs.1,4 Other bacteria associated with UTI
include Staphylococcus, Streptococcus,
Enterococcus, Proteus, and Klebsiella
species.
Risk Factors
- UTI is associated with alterations in the host’s systemic or
local immunity, such as immunosuppression, diabetes,
hyperadrenocorticism, anatomic abnormalities (polyps/tumors,
recessed vulva), indwelling catheters, uroliths, or urethral
sphincter mechanism incompetence.
- In cats, risk factors include diabetes mellitus,
hyperthyroidism, and renal disease.2
Pathophysiology
- E coli is considered a normal component of
gastrointestinal and distal urogenital flora, but it can ascend
the urethra and gain entrance to the urinary tract. Hematogenous
spread is uncommon.
- Specific virulence factors found in E coli allow it
to adhere to and invade host cells, produce toxins, utilize host
nutrients, and evade the host’s immune system.
Signs
► Thorough medical history, including details
of previous UTI, current or recent medications, and response to
treatment, is essential.
► Patient history for UTI typically includes changes in urination
(amount, frequency, color, straining). Pollakiuria, stranguria,
hematuria, and malodorous urine may indicate cystitis. Dogs with
pyelonephritis or prostatitis may have polyuria/polydipsia and signs
of systemic illness, such as lethargy, anorexia, and vomiting.
► Some dogs have silent UTIs with no urinary signs, although they
may have evidence or history of concurrent disease.
►Findings on physical examination may be
normal in simple UTI.
►Thorough examination for complicated UTI should include abdominal
palpation for hepatomegaly, renal pain, thickened bladder wall, and
cystouroliths; rectal palpation for prostatomegaly, urethral
uroliths, and thickened urethra; and external examination for
recessed vulva (Figure 1).

Figure 1. A 1-year-old golden
retriever with recessed vulva and evidence of skinfold pyoderma is
prepared for episioplasty. Photo courtesy of Emily Klocke, DVM,
Diplomate ACVS
DIAGNOSIS
Definitive
- Urine culture and susceptibility testing, preferably on a
sample obtained by cystocentesis or urinary catheter, are
definitive for UTI. Other methods of collection require a
quantitative culture to rule out contamination.
Differential
- While infection with E coli is most common, many
bacteria, including Staphylococcus, Streptococcus,
Enterococcus, Proteus, and Klebsiella
species, may be responsible. Fungal organisms can also cause UTI.
Laboratory Findings
- Complete blood count will be within the reference intervals
and is not required for diagnosis of simple UTI. However, an
increase in white blood cells may be present with pyelonephritis
or prostatitis.
- Serum biochemical profile will show abnormalities consistent
with the underlying disease (chronic kidney disease,
hyperadrenocorticism) in complicated UTI.
- Pyuria, bacteriuria (Figure 2), hematuria,
or proteinuria may be noted on urinalysis.
Figure 2. Canine uirine sediment prepared as an
unstained wet mount (A) and with modified Wright's
stain (B) showing numerous bacilli and leukocytes
(40x magnification). Courtesy of Don Peterson, DVM
Figure 2a
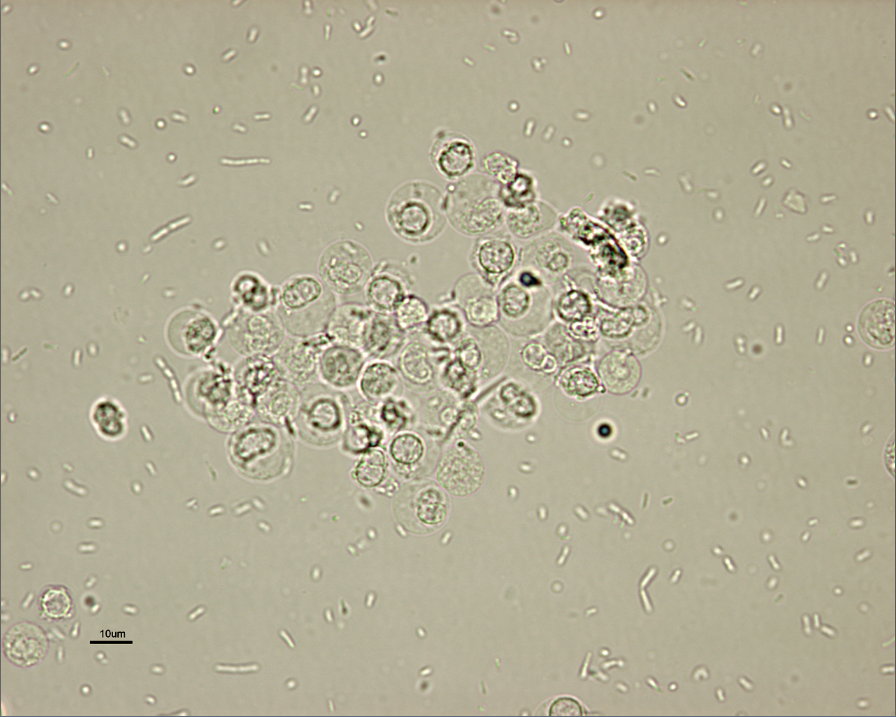
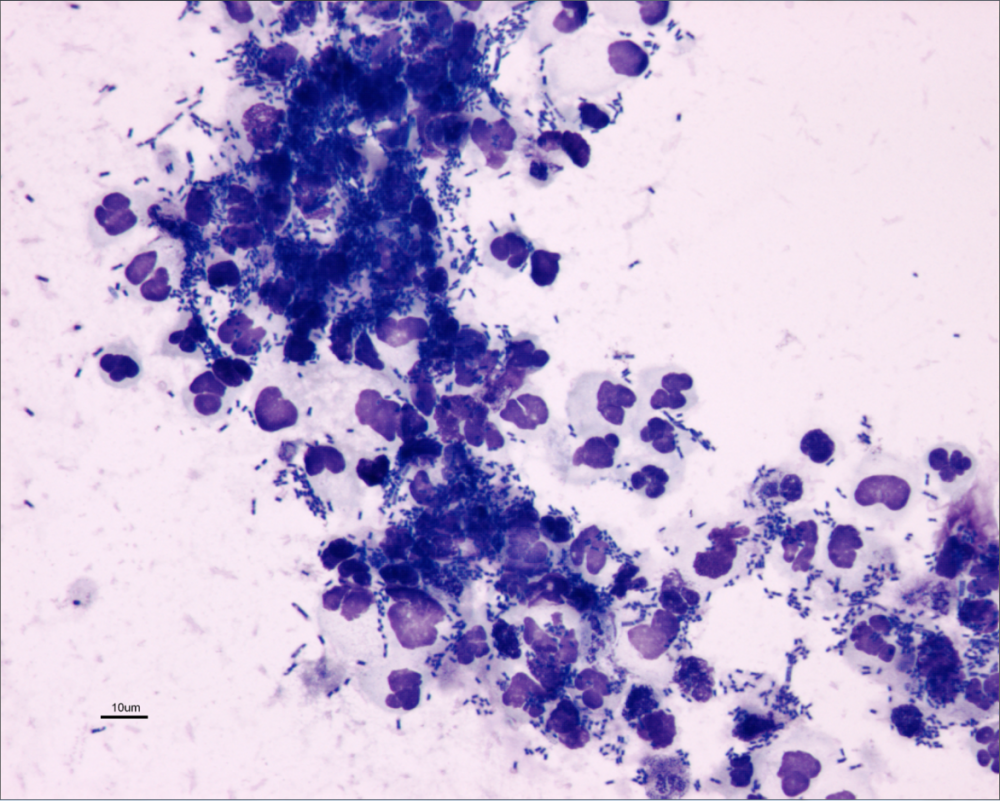
Figure 2b
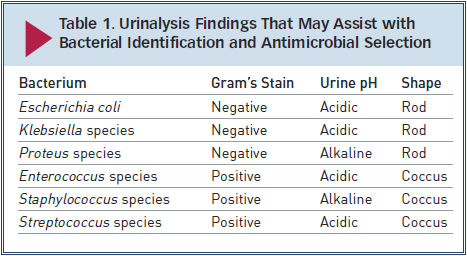
► Gram’s staining and measurement of urine pH
may help narrow the differential diagnosis while culture is pending
(Table 1). However, urine pH may be affected by
other factors (fasting versus postprandial, diet, renal disease,
vomiting, drugs).
► Not all cases of UTI have active urine sediment; immunosuppression
can block the local inflammatory response.
- Minimum inhibitory concentrations (MICs) should be requested
for culture and susceptibility testing of urine.
- Evaluation of endocrine function is indicated if suggested
by clinical presentation (measurement of serum thyroxine
concentration in a cat with polyphagia, weight loss, and
palpable thyroid nodule).
Imaging
- For complicated UTI, radiography and ultrasonography are
indicated for assessment of uroliths, pyelonephritis (Figure
3), prostatitis, adrenomegaly, or other complicating
factors. Contrast studies or cystoscopy may be indicated to
investigate anatomic defects.
A.

B.

Figure 3. Longitudinal (A) and transverse (B)
renal ultrasound images of an 8-year-old female domestic shorthaired
cat with pyelonephritis. These images show dilation of the renal
pelvis, which is characteristic of pyelonephritis.
TREATMENT
- Simple versus complicated infections, location of infection,
susceptibility of strain, adverse effects of antimicrobial
agents, and client compliance issues should be evaluated prior
to treatment for E coli infections.
- Most patients are treated as outpatients, but patients with
pyelonephritis or prostatitis due to infection with E coli
may benefit from hospitalization and supportive care.
► Most infections can be effectively managed
or cured with appropriate antimicrobial treatment, but episioplasty
may be indicated in female dogs with a recessed vulva. Surgery or
lithotripsy for uroliths or surgical resection of polyps/tumors
should be performed when possible.
- Concurrent conditions should be identified and managed
appropriately to minimize risk for UTI recurrence.
Antimicrobials
- Complete 10- to 14-day course for simple UTI or 4 to 6 weeks
for complicated UTI.
► Empirical antimicrobial selection can be
based on urinalysis findings for simple UTI. Most E coli
strains are susceptible to amoxicillin, amoxicillin–clavulanic acid,
or cephalexin. Enrofloxacin should be avoided as first-line
treatment because of resistance.5
► Antimicrobial choice for complicated UTI should be based on
culture and susceptibility testing and the ability of the drug to
achieve more than 4 times the reported MIC in urine.
► A lipid-soluble antimicrobial agent that can cross the
blood–prostate barrier, such as enrofloxacin, chloramphenicol, or
trimethoprim–sulfamethoxazole, is recommended for prostatitis.
Castration should be performed after acute inflammation resolves.
Supportive Treatment
- Some supportive treatments prescribed in conjunction with
appropriate antimicrobial treatment and monitoring (Table
2) may be suitable for patients with recurrent E
coli UTI.
- Note: Further research is required to
determine efficacy, safety, and optimal dosing profiles for
these treatments in companion animals.
► Methenamine is a urinary antiseptic
that is converted to formaldehyde and can have bactericidal activity
against E coli.6 Methenamine is often
administered with a urinary acidifier; however it is contraindicated
in dogs with metabolic acidosis (chronic kidney disease, diabetic
ketoacidosis) and is not well tolerated by cats.
► Proanthocyanidins (found in cranberries) can prevent
E coli adhesion to the uroepithelium.7 Preliminary
research suggests cranberry extract has antiadhesive effects in
canine urine.8,9
► D-mannose is a sugar that competitively binds to
mannose-sensitive fimbriae on E coli, which can inhibit
adhesion to or displace adhered E coli from the
uroepi-thelium.10
► Forskolin is the main active ingredient in the Asiatic
herb Coleus forskohlii and may stimulate exocytosis of
E coli from the urinary bladder wall.11 It may be
useful in relapsed UTI with suspected poor antimicrobial
penetration.

FOLLOW-UP
Patient Monitoring
- Optimal monitoring for complicated and recurrent UTI
includes urine culture 3 to 5 days after initiation of
treatment.
► No growth on culture suggests effective
treatment.
►Growth on culture suggests ineffective treatment, and antimicrobial
choice should be reconsidered.
- Bacterial culture should be negative prior to
discontinuation of treatment and again 5 to 7 days following
discontinuation of antimicrobial treatment.
Recurrence and Resistance
- Recurrence of UTI with the same organism warrants further
investigation of potential problems with antimicrobial treatment
and/or reevaluation for a source of the infection (uroliths or
neoplasia).
- Recurrence of UTI with a different organism warrants further
investigation for a cause of immunosuppression.
- Preventive low-dose antimicrobial treatment (eg,
nitrofurantoin 4 mg/kg PO once at bedtime instead of Q 8 H) may
be indicated for recurrent E coli UTI with an
identifiable underlying cause. Low-dose treatment should be
initiated after the current infection is properly controlled
(following 4–6 weeks of antimicrobial treatment at the
therapeutic dose and a negative urine culture).
IN GENERAL
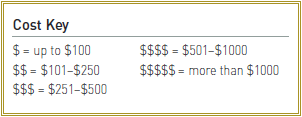
Relative Cost
►The cost for a physical exam, urinalysis, +/-
urine culture & susceptibility, and cost of antimicrobial treatment:
$-$$
►The total expense for initial extensive diagnostic testing,
antimicrobial treatment, and multiple follow-up cultures can be
costly: $$$-$$$$
UTI = urinary tract infection
From
Clinician's Brief


